Expand all
Collapse all
Overview
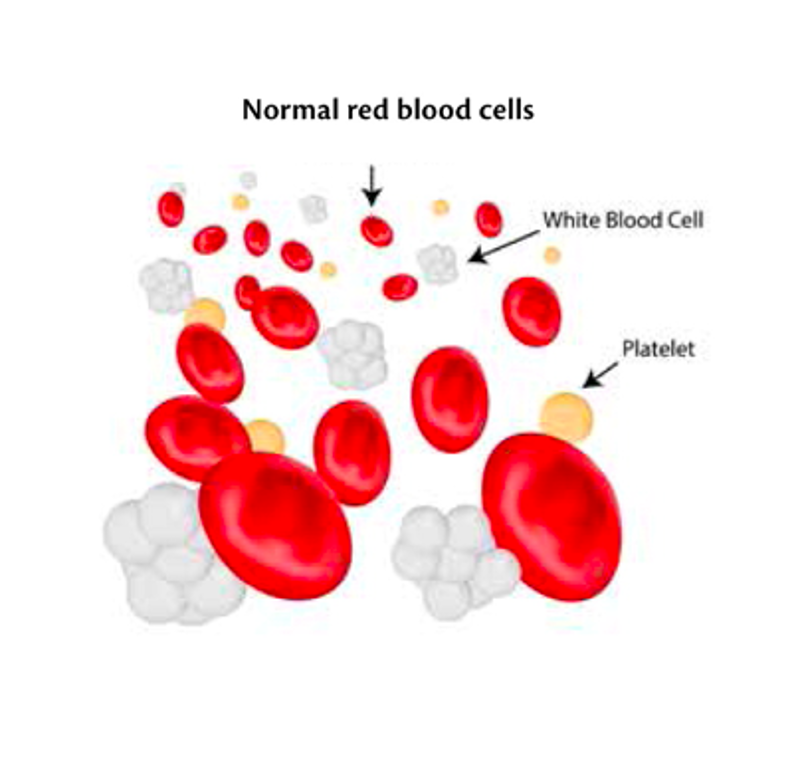
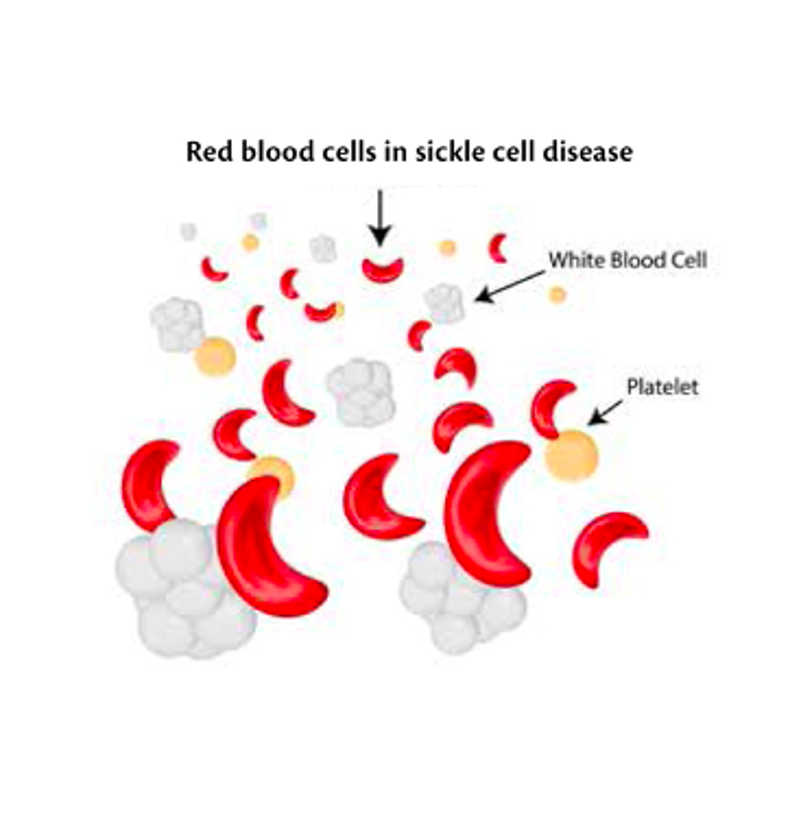
Sickle cell disease predominantly affects people of African, Caribbean, Middle Eastern, Eastern Mediterranean and Asian origin. People with sickle cell disease produce abnormally shaped red blood cells that can become rigid (Figure 1). The crescent shape forms because of abnormalities in the haemoglobin inside the cell. These sickle-shaped cells do not live as long as healthy blood cells and they can become stuck in blood vessels, causing acute painful sickle cell episodes (National Institute for Health and Care Excellence (NICE), 2012).
To view the rest of this content please log in
Symptoms
Most children with sickle cell disease have few symptoms in early childhood and mostly lead normal lives. However, some children experience problems early on in the disease. The main symptoms of sickle cell disease include the following (NICE, 2012; 2021):
Sickle cell crisis
These are painful episodes lasting up to a week and are one of the most common symptoms of sickle cell disease. It occurs when blood vessels to parts of the body become blocked, often occurring in a particular part of the body such as hands, feet, spine, abdomen or a limb. The pain can be severe enough to require hospital admission. Frequency of episodes varies from sufferer to sufferer, but the average is one severe episode a year. The trigger of the episodes may not always be identified but can be caused by weather (e.g. wind, rain or cold), dehydration, stress or strenuous
To view the rest of this content please log in
Aetiology
Sickle cell disease is caused by a faulty gene that affects how red blood cells develop. If both parents carry this sickle cell trait, there is a 1 in 4 chance of each child they have being born with sickle cell disease. If both parents are carriers, there is a 1 in 2 chance that each baby will also be a carrier of the sickle cell trait. The trait is identified through a simple blood test, which is done during pregnancy, and is part of the newborn blood spot test. However, anyone can request to have the test to establish if they are a carrier (NICE, 2021).
To view the rest of this content please log in
Management
People with sickle cell disease need specialist care throughout their lives. Treatments and preventive care include the following (NICE, 2012; 2021):
- For painful episodes:
- staying hydrated
- wearing warm clothing in bad weather
- heat pads and gentle massage in the painful areas
- avoiding sudden temperature changes such as swimming and cold weather
- initially, pain is treated with simple analgesia such as paracetamol and ibuprofen. However, stronger pain killers such as morphine are often needed and sufferers are frequently admitted to hospital for pain management
- hydroxycarbamide is sometimes prescribed. It is a drug that reduces the number of blood cells produced by bone marrow.
- For reducing the risk of infections:
- adherence to the full vaccination programme as well as the uptake of additional vaccines, such as the flu vaccine and hepatitis B
- a daily dose of antibiotics, usually penicillin, often for the rest of their life.
- For anaemia:
- dietary supplements such as folic acid may
To view the rest of this content please log in
Treatment
Stem cell or bone marrow transplants can potentially cure sickle cell disease, but they are not done very often because of the significant risks involved, such as graft vs host disease, which can be fatal. Stem cell transplants are usually only considered in children with severe symptoms that do not respond well to other treatments (NICE, 2021).
Many children with sickle cell disease will lead relatively normal lives, but some of the complications of the disease, such as strokes and serious infections, can be life threatening or even fatal. Overall, the life expectancy for someone with sickle cell disease is shorter, but varies depending on the type of sickle cell disease they have, how it is treated and what complications arise. The current average life expectancy is between 40 and 60 years of age. Some of the milder types of sickle cell disease may have no impact on life expectancy.
To view the rest of this content please log in
Resources
References
National Institute for Health and Care Excellence. Sickle cell disease: managing acute painful episodes in hospital. 2012. www.nice.org.uk/guidance/cg143 (accessed 13 January 2022)
National Institute for Health and Care Excellence. Sickle cell disease. 2021. https://cks.nice.org.uk/sickle-cell-disease#!topicsummary (accessed 10 January 2023)
Sickle Cell Society. About Sickle Cell. 2023. www.sicklecellsociety.org/about-sickle-cell/ (accessed 10 January 2023)
To view the rest of this content please log in