Foot care for people with diabetes
Foot ulceration is the foremost cause of hospital admission in people with diabetes. Foot ulcers are prone to rapidly spreading infection, resulting in overwhelming tissue destruction and often necessitating major amputation.
Article by Jayne Robbie
Expand all
Collapse all
Overview
Foot ulceration is the foremost cause of hospital admission in people with diabetes, with the incidence of wound infection on initial presentation having increased in recent years. Foot ulcers are prone to rapidly spreading infection, resulting in overwhelming tissue destruction and often necessitating major amputation. Amputations are not only limb threatening but also life limiting, as only around 50% of patients survive for 2 years after major amputation occurring as a result of diabetes.
The importance of multi professional working and robust care pathways ensures that patients have access to the right medical interventions at the optimum time, demonstrating that early referral to specialist care reduces amputation rates and times to healing, and that multi-professional teamwork (inpatient and community-based or outpatient) can reduce both hospital admissions and amputation rates.
To view the rest of this content login below; or read sample articles.
Purpose
Foot ulcers in people with diabetes are complex and often chronic wounds, which can have major long-term implications for the morbidity, mortality and quality of life (Vainieri et al, 2020). They are frequently life changing and limb threatening, as one in three people with diabetes can develop foot ulcers in their lifetime (Armstrong et al, 2017). Kerr (2017) noted that people with diabetes are approximately 23 times more likely to have a toe, foot or limb amputated than those without the condition, representing a significant challenge for both primary and secondary care services.
Foot infection is the most common complication of diabetes requiring acute admission to hospital as well as being the most common cause of non-traumatic lower limb amputation (National Institute for Health and Clinical Excellence, 2002).
To view the rest of this content login below; or read sample articles.
Assessment
Foot ulcer risk assessment
Community services are increasingly at the forefront of caring for people with diabetes, and an essential part of that care involves foot screening in order to determine the risk of ulceration (Rawles, 2014), as it has been suggested that as much as 80% of diabetes-related amputations are avoidable (Diabetes UK, 2019).
How to perform a foot check
When carrying out a foot check, practitioners should take a comprehensive diabetes history, then carry out the following assessment:
- remove shoes and socks/stockings
- test foot sensations using 10g monofilament or vibration with a tuning fork or Ipswich Touch Test
- palpate foot pulses
- inspect for any deformity or discolouration
- inspect for significant callus
- check for signs of ulceration
- ask about any previous ulceration
- inspect footwear
- tell patient how to look after their feet and provide written information
- tell patient their risk status and what it means
- explain what to look
To view the rest of this content login below; or read sample articles.
Procedure
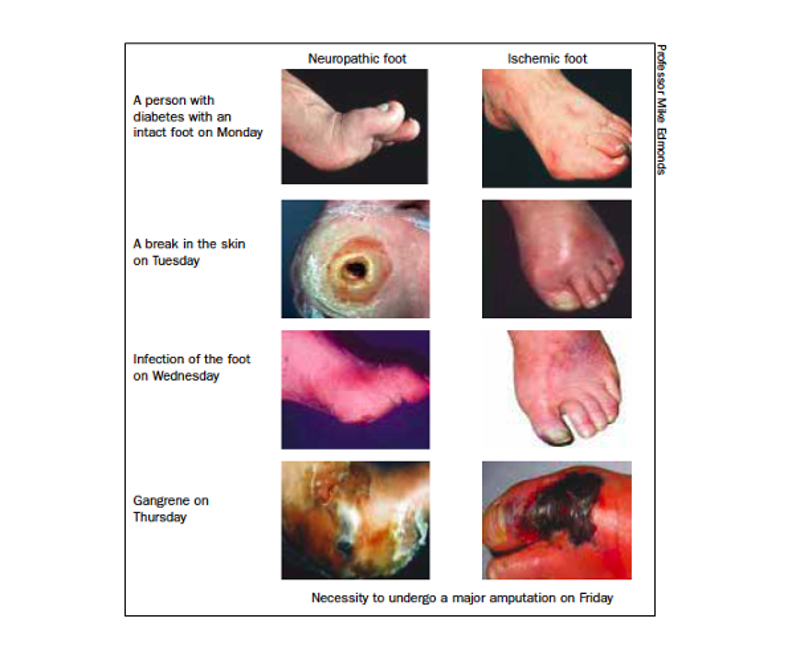
There are predominately two types of foot ulcers in diabetes (Table 2): neuropathic ulcers which occur in patients with a loss of peripheral pain sensation (Figure 3) and ischaemic ulcers which occur in people with a deficient blood supply to the extremities (Figure 4).


|
Table 2. Comparison of neuropathic and ischaemic ulceration |
|
| Neuropathic | Ischaemic |
|
Generally good blood supply Limb/foot usually warm/pink Bounding pulses |
Evidence of peripheral arterial disease Limb/foot may be cool/pale |
To view the rest of this content login below; or read sample articles.
Risks and complications
Infection is common across all types of ulceration, often spreading rapidly through the foot and causing major tissue destruction (Figure 6).

The signs of a red, hot, swollen foot should not be underestimated, as the progression from an initial relatively minor injury to unsalvageable tissue necrosis and overt gangrene can take as little as 48 hours (Figure 7) (Edmonds et al, 2020).
Early recognition of this serious situation is essential
To view the rest of this content login below; or read sample articles.
Next steps
iDEAL recommends that the assessment tool should be used for all people with diabetes who present:
- with any foot problem
- by all practitioners
- in all locations and
- that the initial foot assessment should be in primary or community care or through community podiatry, or community nursing
- with referral made by telephone or email to the multidisciplinary diabetes foot care teams (with as much supporting information) if required (Edmonds et al, 2020)
Use of the ACTNOW assessment tool will ensure consistency in each individual assessment, as the individual clinician’s skill and judgement regarding the need for escalation to a specialist centre will as a result of a structured clinical history and examination as well as their own experience.
Additional red flag indicators should be noted, which necessitate the need for urgent referral to a specialist clinic for further assessment and treatment:
To view the rest of this content login below; or read sample articles.
NMC proficiencies
Nursing and Midwifery Council: standards of proficiency for registered nurses
Part 2: Procedures for the planning, provision and management of person-centred nursing care
3.1 observe and assess comfort and pain levels and rest and sleep patterns
4.1 observe, assess and optimise skin and hygiene status and determine the need for support and intervention
9.1 observe, assess and respond rapidly to potential infection risks using best practice guidelines
To view the rest of this content login below; or read sample articles.
Resources
Armstrong DG, Boulton AJ, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med. 2017;376:2367-2375. https://doi.org/10.1056/NEJMra1615439
Diabetes UK. Number of people with diabetes reaches 4.7 million. 2019. https://www.diabetes.org.uk/about_us/news/new-stats-people-living-with-diabetes (accessed 29 November 2023)
Edmonds ME, Foster AVM. Managing the diabetic foot. 3rd edn. Wiley Blackwell: Oxford; 2014
Edmonds ME, Phillips A, Grumitt J et al. iDEAL group position statement: ACT NOW! Diabetes foot care and referral. 2020. https://idealdiabetes.com/wp-content/uploads/2020/11/iDEAL-Diabetes-ACT-NOW-Diabetes-and-Foot-Health.pdf (accessed 29 November 2023)
Kerr M. Diabetic foot care in England: an economic study. 2017. https://diabetes-resources-production.s3-eu-west-1.amazonaws.com/diabetes-storage/migration/pdf/Diabetic%2520footcare%2520in%2520England%2C%2520An%2520economic%2520case%2520study%2520(January%25202017).pdf (accessed 29 November 2023)
Kinlay, S. Management of critical limb ischemia. Circulation: Cardiovascular Interventions. 2016;9(2). https://doi.org/10.1161/CIRCINTERVENTIONS.115.001946
Miller JD, Carter E, Shih J et al. How to do a 3-minute diabetic foot exam. J Family Practice 2014; 63(11): 646–56
National Institute for Health and Clinical Excellence. Principles for best practice in clinical audit. 2002. https://www.nice.org.uk/media/default/About/what-we-do/Into-practice/principles-for-best-practice-in-clinical-audit.pdf (accessed 29 November 2023)
Phillips A, Edmonds M. ACT NOW in diabetes and foot assessments: an essential service. Br J Community Nurs. 2021; 26(3):116-120.
To view the rest of this content login below; or read sample articles.